Carvykti™, the new advanced therapy approved by FDA
INTRODUCTION
¹. CARVYKTI™ (ciltacabtagene autoleucel – Johnson & Johnson) was approved by the U.S. Food and Drug Administration (FDA) in February 2022 for the treatment of relapsed or refractory multiple myeloma after four or more prior lines of therapy, including proteasome inhibitors, immunomodulators, and anti-CD38 monoclonal antibodies. The disease is a blood cancer that affects plasma cells, found in the bone marrow. When damaged, these cells quickly spread and give rise to tumors. Although additional treatment options have been developed in recent years, most patients with multiple myeloma face a poor prognosis after disease progression following treatment with these three primary therapy classes².
DRUG CHARACTERISTICS
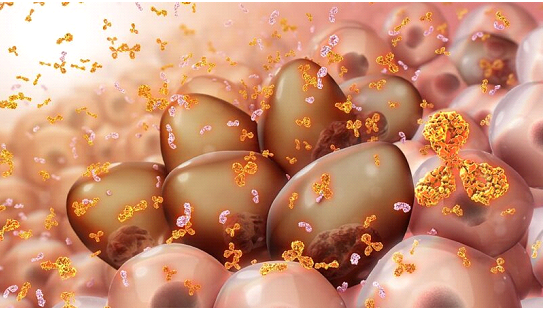
CARVYKTI™ is a chimeric antigen receptor T-cell (CAR-T) therapy using two single-domain antibodies directed against B- cell maturation antigen (BCMA). It involves reprogramming a patient’s own T cells with a transgene encoding a chimeric antigen receptor (CAR) that recognizes and eliminates BCMA-expressing cells. Malignant B cells of multiple myeloma are the cells that mainly express BCMA, although mature B cells and plasma cells do it too. When bound with BCMA-expressing cells, the therapy promotes T cell activation, expansion, and elimination of target cells2.
APPROVAL
The approval of the therapy was based on data from the pivotal, open-label, multicenter, Phase 1b/2 CARTITUDE-1 study, which enrolled patients with a median of six prior regimens and whose disease progressed during or after the last treatment. Previous treatment regimens included at least one proteasome inhibitor, one immunomodulator, and one anti-CD38 monoclonal antibody. Of the 97 patients enrolled in the study, 99% were refractory to last-line therapy, and 88% were triple-class refractory, meaning their cancers did not respond, or no longer respond, to any of the three main treatment categories. In the CARTITUDE-1 clinical study, 98% of patients with relapsed or refractory multiple myeloma responded to ciltacabtagene autoleucel monotherapy, and 78% of responders experienced a strict complete response. Responses showed durability over time, resulting in most heavily pretreated patients achieving deep responses at 18 months of follow-up2.
RISK ASSESSMENT
As a personalized medicine, CARVYKTI™ treatment requires extensive training, preparation, and certification to ensure a positive patient experience. It is only available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the CARVYKTI™ REMS program. Safety information for this therapy includes a warning on Cytokine Release Syndrome, Immune Effector Cell-Associated Neurotoxicity Syndrome, Parkinson’s disease, Guillain-Barré syndrome, hemophagocytic lymphohistiocytosis/macrophage activation syndrome, and persistent or recurrent cytopenia2.

Need more information? Talk with us
Looking for project funding? Talk with us
REFERENCES
1. FDA grants approval to Janssen’s Carvykti for multiple myeloma treatment.
2. U.S. FDA Approves CARVYKTITM (ciltacabtagene autoleucel), Janssen’s First Cell Therapy, a BCMA-Directed CAR-T Immunotherapy for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma | Johnson & Johnson. Content Lab US. .
Carvykti™, the new advanced therapy approved by FDA
Carvykti™, the new advanced therapy approved by FDA
Share This Post
More To Explore

Tecartus
INTRODUCTION Tecartus is a new advanced therapy approved to treat adults with mantle cell lymphoma (MCL)¹. This disease is a lymphatic system cancer. Specifically, it

KYMRIAH, AN ANTI-CD19 CAR-T THERAPY
INTRODUCTION Kymriah (Novartis) is an advanced therapy medicine that belongs to the gene therapyproduct category. It is approved for B-cell acute lymphoblastic leukemia (ALL) in